Diagnosis of acute rhinosinusitis in primary care: a systematic review of test accuracy
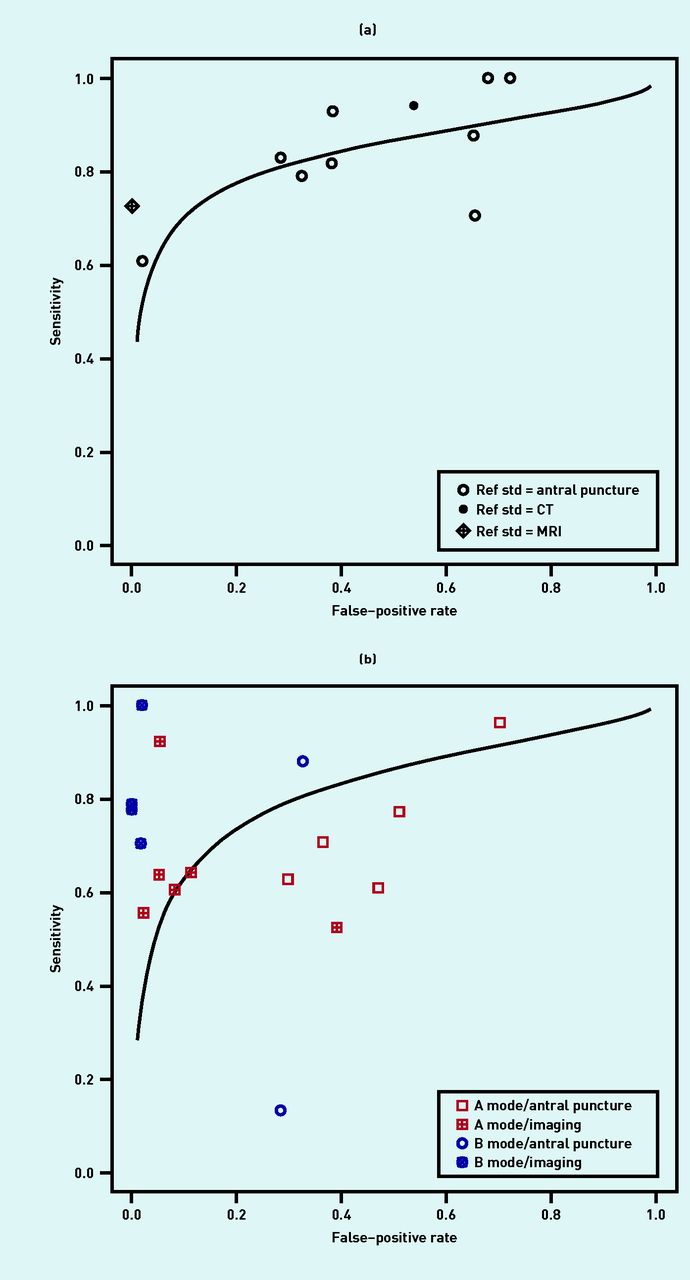 Image credit: BJGP
Image credit: BJGP
Abstract
Acute rhinosinusitis (ARS) is a common primary care infection, but there have been no recent, comprehensive diagnostic meta-analyses. To determine the accuracy of laboratory and imaging studies for the diagnosis of ARS. Systematic review of diagnostic tests in outpatient, primary care, and specialty settings. The authors included studies of patients presenting with or referred for suspected ARS, and used bivariate meta-analysis to calculate summary estimates of test accuracy and the area under the receiver operating characteristic (ROC) curve. The authors also plotted summary ROC curves to explore heterogeneity, cutoffs, and the impact of different reference standards. Using antral puncture as the reference standard, A mode ultrasound (positive likelihood ratio [LR+] 1.71, negative likelihood ratio [LR−] 0.41), B mode ultrasound (LR+ 1.64, LR− 0.69), and radiography (LR+ 2.01, LR− 0.28) had only modest accuracy. Accuracy was higher using imaging as the reference standard for both ultrasound (LR+12.4, LR− 0.35) and radiography (LR+ 9.4, LR− 0.27), although this likely overestimates accuracy. C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) both had clear threshold effects, and modest overall accuracy. The LR+ for ESR >30 and >40 were 4.08 and 7.40, respectively. A dipstick of nasal secretions for leucocyte esterase was highly accurate (LR+ 18.4, LR− 0.17) but has not been validated. In general, tests were of limited value in the diagnosis of ARS. Normal radiography helps rule out sinusitis when negative, whereas CRP and ESR help rule in sinusitis when positive, although, given their limited accuracy as individual tests, they cannot be routinely recommended. Prospective studies integrating signs and symptoms with point-of-care CRP, dipstick, and/ or handheld B-mode ultrasound are needed.
Supplementary notes can be added here, including code and math .